INTRACRANIAL DYNAMICS
AND SHUNT TECHNOLOGY
RESEARCH STRATEGY
Background
Intracranial dynamics focuses on the mechanism and models of the blood supply to the brain and its buoyancy mechanism. How do changes in cerebral blood flow (CBF) and the cerebrospinal fluid (CSF) circulation interact in time and in space and how may stable flows and fluxes be preserved over a wide range of compartmental pressures with the brain? How do such control systems change with brain injury and how may such disturbances be ameliorated?
Cerebral autoregulation (CA) controls and adapts cerebral blood flow (CBF) over a range of cerebral perfusion pressures (arterial blood pressure minus intracranial pressure) thereby ensuring adequate perfusion and oxygenation of the brain. This crucial neuroprotective mechanism, which provides the haemodynamic reserve to cope with various insults, is variably impaired following acute brain injury in newborn infants, children and adults, and is an independent predictor of poor outcome.

Significant advances in TBI outcome have been achieved over the last 20 years by brasing our management of systemic and cerebrovascular physiology on targets derived from population studies. However, this approach takes no account of interpatient heterogeneity as reflected by varying degrees of autoregulatory reserve in different patients and its time-variability.
There is mounting evidence that including cerebral autoregulation in the ICU management of patients after severe TBI is beneficial to patient’ survival and generally better outcome. Autoregulation based individualisation of therapy thresholds has been included in the recent brain trauma guidelines. However there are still no clinically approved monitors of cerebral autoregulation available.
Crucial to such studies has been the development of techniques for the continuous monitoring of cerebrovascular reactivity [Czosnyka M, Stroke 1996] and cerebral autoregulation [Czosnyka M, Neurosurgery 1997]. These novel methods, based on computer-supported time-series analysis were introduced in 1996-1997 and have demonstrated such methods can be beneficial in the acute stage of management of TBI patients for the individual optimization of management strategies.
This work led to the development of the concept of defining an individual patient’s ‘Optimal Cerebral Perfusion Pressure’, using continuous monitoring of a dynamic index of cerebral autoregulation [Steiner L Critical Care Medicine 1997] – until this work, patients were assumed to require the same cerebral perfusion pressure.
Aims and specific short (1 year), medium (2-3 years) and long (4-5 years) objectives
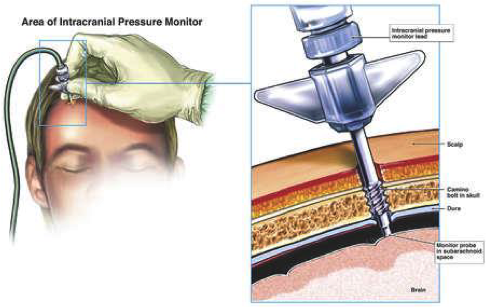
- A new method based on combined measurements of optic nerve sheath diameter and venous Doppler blood flow velocity will be validated against invasive monitoring of ICP
- Computing tools for targeted management of CPP in TBI patients will be developed for ICM+ software
- Cambridge Shunt Evaluation Laboratory – assessment of the Certas 2 valve
- A monitoring cart will be designed for non-ivasive brain monitoring, containing TCD ultrasonograph, plethysmographic arterial blood pressure monitor and profiled custom version of ICM+ to assess multiple parameters of brain circulation, including autoregulation, critical closing pressure, diastolic closing margin, and baraoreflex sensitivity
- Near infrared Spectroscopy will be added to the cart to facilitate assessment of ‘optimal’ arterial blood pressure target
- A multicenter RCT is planned to assess the efficacy of the ‘optimal CPP’ approach to management of TBI
- Creation of a comprehensive multimedia support to improve dissemination of the knowledgebase pertaining to the CSF dynamics investigatigative suite of tools implemented in ICM+. This will be made available on-line via a new, redesigned ICM+ web portal.
- Diffuse Correlation Spectroscopy is a new technique using near infrared light, able to monitor CBF in absolute units (ml/min/100g). We plan to add and validate DCS using the non-invasive brain monitoring platform
- Continuation of ‘optimal CPP’ trial.