FUNCTIONAL NEUROIMAGING
AND NEUROPHYSIOLOGY
RESEARCH STRATEGY
Aims and specific short (1 year), medium (2-3 years) and long (4-5 years)
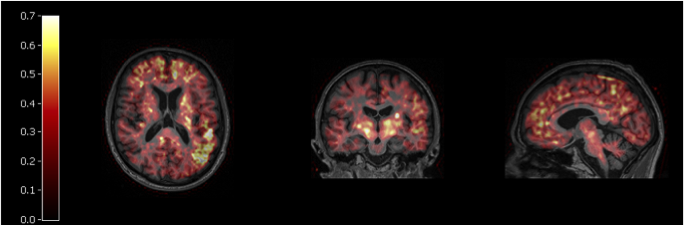
- Establish quantitative PET-MR imaging methods
- Establish clinical imaging of synaptic density
To facilitate wider exploitation and enable lower cost for PET radiotracers we develop a novel method for manufacture based on flow chemistry using a patented micro Capillary films in collaboration with Prof Nigel Slater (Dept. of Chemical Engineering and Biotechnology).
Subthemes
Over the past 5 years, two tracers (11C-methionine and 11C-metomidate) have transformed the care of subgroups of patients with pituitary and adrenal tumours who were previously deemed unsuitable for surgery, and who had often been consigned to a lifetime of expensive/poorly tolerated medical treatment, are, in many instances, undergoing curative surgery.
For example, a single 11C-methionine scan costing £1250 may facilitate curative trans sphenoidal surgery (£6,500), allowing the discontinuation of drugs (e.g. somatostatin analogues such as lanreotide Autogel or Sandostatin LAR) costing >£10,000 per annum, thus not only improving quality of life, but also producing considerable costs savings for the NHS (Koulouri et al Eur J Endocrinol 2016, 175(5):485-498. PMID: 2756240; Koulouri et al Eur J Endocrinol, 2015, 173(4):M107-20 PMID: 26245763). Similarly, in primary aldosteronism (which is now recognised to be the commonest secondary cause of hypertension (5-10% of all cases and 20- 25% of refractory hypertension), 11C-metomidate PET-CT has facilitated curative surgery (unilateral adrenalectomy) in patients who have previously had failed adrenal vein sampling and were therefore unable to proceed further along the surgical pathway (Burton et al 2012. J Clin Endocrinol Metab, 97(1):100- 9. PMID: 22112805). Currently, Dr Gurnell is processing 3-5 new referrals every week from around the UK and overseas – including Europe, USA and even Australia without even advertising the service. The pituitary PET studies were initially funded from JDP’s NIHR senior investigator award and substantial funding has now followed (NIHR EME, MRC DPFS and Evelyn Trust awards). Novel tracers for these patient groups are being explored together with health economic issues around such a ‘disruptive technology’ with the aid of methods such as decision analytic models (Drummond MF, Methods for the Economic Evaluation of Health Care Programmes, Oxford University Press, 2005; Heinzel et al J Nucl Med. 2013).
We have conducted commercial and non commercial testing of medical devices for safety in the MR environment which will now be extended to 7T: intracranial pressure transducers, ventilators, infusion pumps, shunts and embolism devices. We have developed non-invasive measurement of brain tissue (and other tissue) compliance/stiffness in collaboration with the University of Edinburgh. patient motion – we have used both MR sequence (radial imaging) and marker based techniques to mitigate the effects of patient motion. Resolution (e.g 1mm isotropic) diffusion imaging including the brain stem has been developed and is of particular relevance to furthering our understanding of the neuroanatomy of the late sequelae of TBI. Brain 31P spectroscopy to assess energy status has been implemented to compliment studies using intracerebral microdialysis (see multimodality monitoring theme).
Functional magnetic resonance imaging (fMRI) and PET have been very successful in measuring cognitive function and even covert awareness in patients who are apparently in a vegetative state but such scanners are often unavailable, expensive or simply infeasible for universal deployment to aid clinical decision-making in the community setting. Requiring patients to regularly travel to specialist fMRI/PET centres is not realistic and could lead to delays in decision-making relating to their clinical management, all of which is upsetting and expensive. In comparison, electroencephalography (EEG) is a relatively inexpensive and portable tool for measuring electrical brain activity, in addition to being painless and non-invasive. Hence EEG is ideal for longitudinal studies and for bedside use in nursing homes and rehabilitation centres where, for example, patients with prolonged disorders of consciousness are typically discharged to from the acute care setting. Though it lacks the spatial resolution of fMRI, recent advances in the use of functional EEG (fEEG) have shown considerable promise for accurately assessing the integrative brain activity associated with complex cognition and consciousness, without any reliance on compliance behaviour from the patients. Convergent with such evidence from other groups, our research at Cambridge also suggests that fEEG, measured for 10 minutes right at the bedside, can be used to characterise how networks of brain activity are fundamentally reorganised following brain injury. Further, we have shown that key signatures of these networks are correlated with the level of behavioural responsiveness at the bedside, and are remarkably robust in seemingly vegetative patients who nevertheless show signs of hidden awareness, as measured by command- following in the form of tennis imagery detected with fMR. Despite these research advances, fEEG has yet to find implementation in to clinical practice, and in an individual patient’s rehabilitation journey in particular. We have stated to evaluate the feasibility of fEEG for bedside visualisation and assessment of brain networks in a real-world context at long- term neurorehabilitation centres that routinely care for patients in Cambridgeshire. This study will help speed up accurate diagnosis, enable longitudinal assessment of patients, and support family counseling.
